
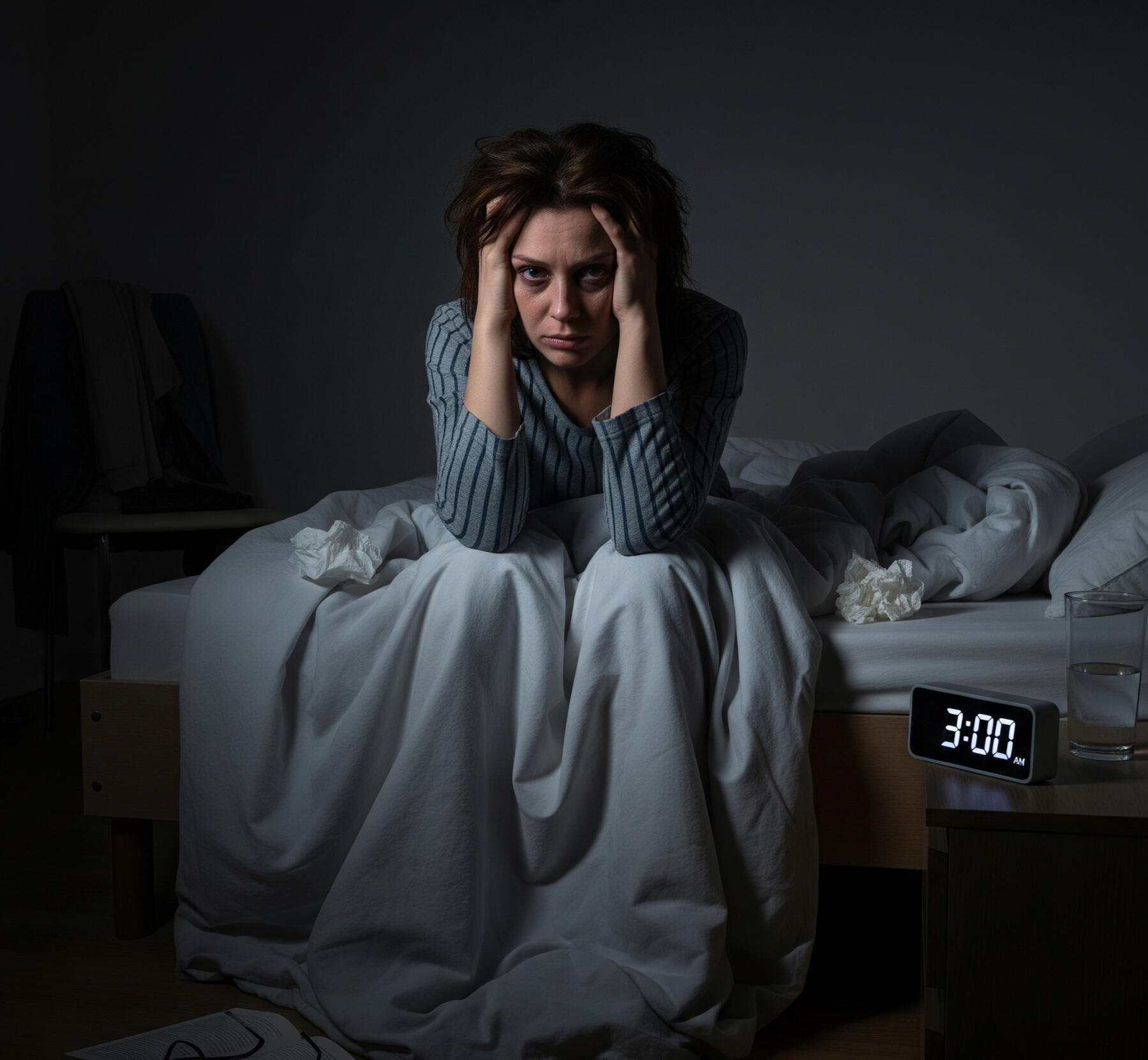
Insomnia + Sleep Apnea = COMISA
Did you know sleep apnea and insomnia often occur together?
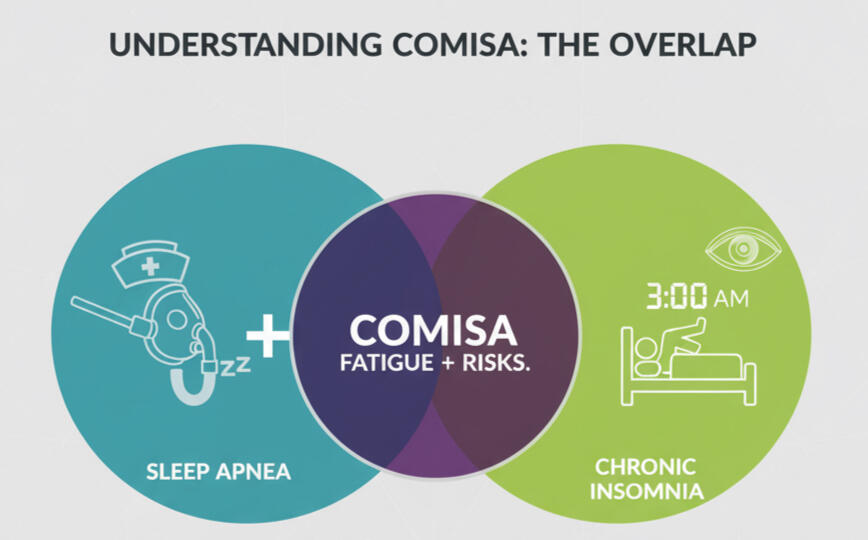
Around 1 in 3 people with either insomnia or sleep apnea actually experience both — a condition called COMISA: Co-Morbid Insomnia and Sleep Apnea.
It’s a widespread but under-recognised condition, affecting millions and possibly hundreds of millions of people worldwide.

Despite being highly prevalent and treatable, insomnia, sleep apnea, and COMISA are widely under-diagnosed.
Up to 80% of sleep apnea cases go undetected
Around 1 in 10 adults experience chronic insomnia
COMISA is often missed or overlooked
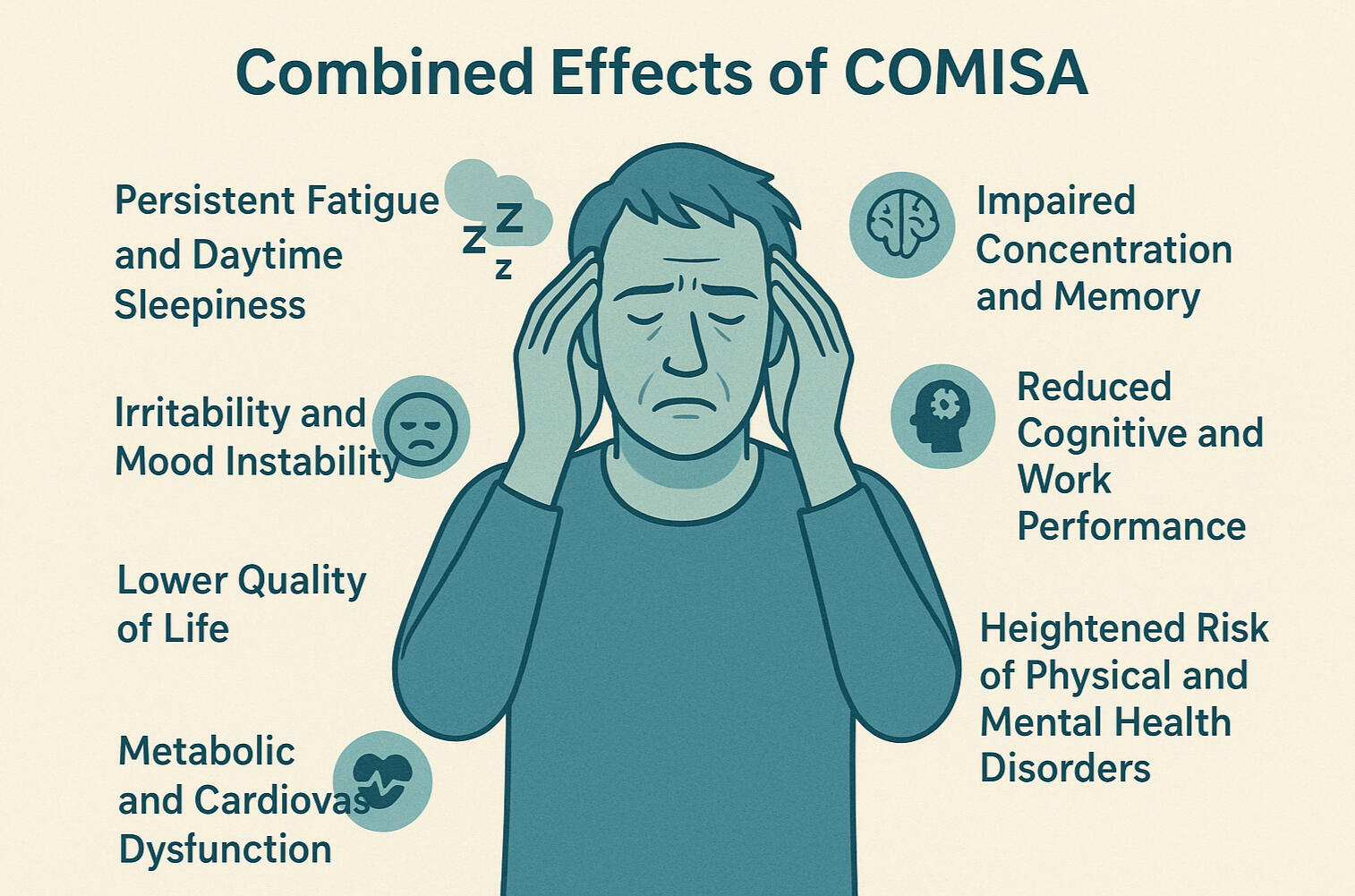
They are hidden epidemics, affecting hundreds of millions worldwide. COMISA poses even greater risks than insomnia or sleep apnea alone.It can lead to serious health and functional impairments:
Poorer sleep quality: more fatigue and reduced daytime performance.
Higher physical health risks: increased risk of heart disease, diabetes, and even early mortality.
Worsened mental health: greater likelihood of stress, anxiety, and severe depression.
If you have symptoms of both insomnia and sleep apnea (COMISA), it's crucial to address both conditions together using a combined approach. .

Download your free COMISA Guide: Breathe. Rest. Repeat.
A Step-by-Step Guide to Managing Insomnia and Sleep Apnea (with CPAP)
Discover proven CBT-i strategies and practical tools you can start using tonight to achieve better, more restful sleep.
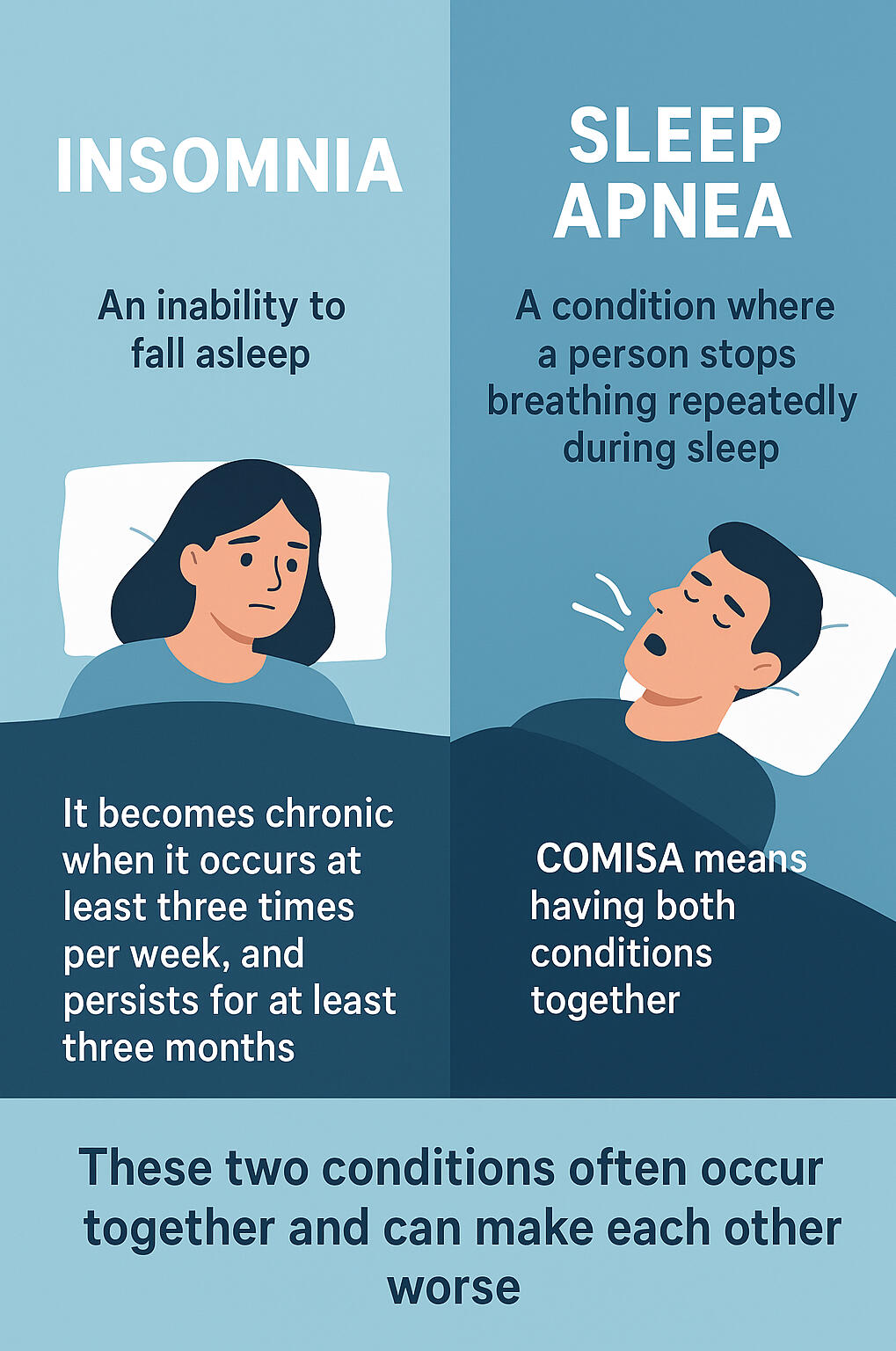
What is COMISA?
COMISA happens when insomnia and sleep apnea overlap. This double challenge makes restful sleep much harder. It's more complex than having either condition alone and is often missed during sleep assessments.
30–50% of sleep apnea patients have insomnia
30–40% of chronic insomnia sufferers have sleep apnea
About 1 in 3 live with both — COMISA
COMISA: When Sleep Disorders Collide
COMISA is more than just poor sleep or two sleep problems at once. It's linked to more serious long-term health risks.
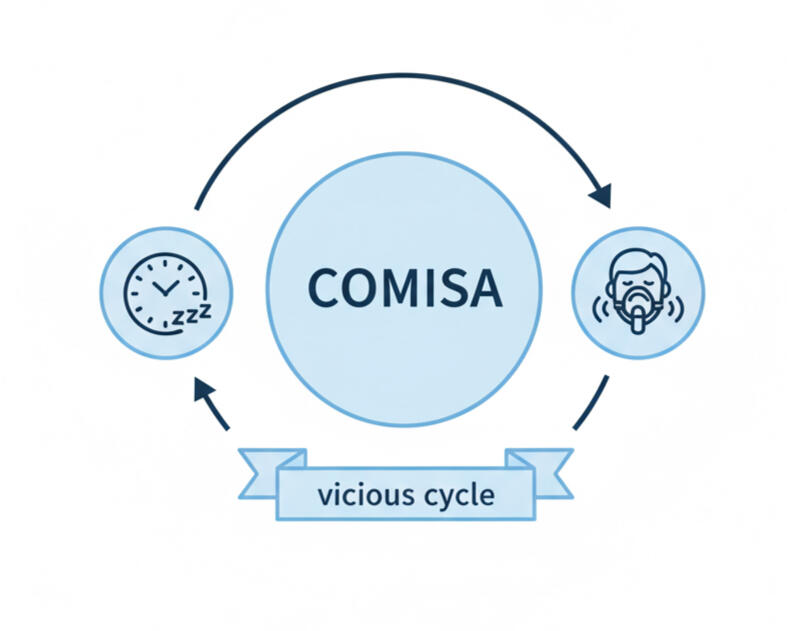
When insomnia and sleep apnea co-occur, they amplify each other’s negative effects. Even if your sleep apnea is treated with CPAP or apnea treatment, co-existing insomnia can still make restful sleep hard to achieve.
Those with COMISA have:
Higher Cardiovascular Risks
Lower Quality of Life
Increased risk of Mood Disturbance
More Difficulties with Treatment — especially CPAP.
50-70% higher risk of Early Mortality
In short, COMISA isn’t just two sleep problems. It’s a serious, compounding condition that requires a coordinated approach.
Sleep apnea causes fragmented sleep, mood changes, and daytime exhaustion.
Insomnia causes difficulty falling or staying asleep, often with anxiety or overthinking at night.
COMISA can make sleep treatments, like CPAP, feel more difficult, intrusive, or uncomfortable.
Check Your Risk
Worried you might have Insomnia? Sleep Apnea? Or both (COMISA)?
Chronic Insomnia: Difficulty falling or staying asleep at least three times per week for three months or longer, despite adequate sleep opportunity.
Sleep Apnea (OSA): Repeated breathing pauses and airway collapse during sleep, causing disrupted sleep and low oxygen levels.
COMISA: The co-occurrence of chronic insomnia and sleep apnea, carrying combined risks and often going undiagnosed.
Take our self-assessments—clinically validated tools designed to help you quickly gauge your risk for insomnia and sleep apnea. If you already have a diagnosis of either condition, these assessments can help identify your risk for COMISA.The Insomnia Severity Index measures insomnia symptoms, while the STOP-BANG and Epworth Sleepiness Scale screen for sleep apnea (often referred to as obstructive sleep apnea or OSA).
Please note: These assessments are for educational purposes only and do not provide a clinical diagnosis.
Insomnia Severity Index (ISI)
STOP BANG Questionnaire
Epworth Sleepiness Scale
Understanding Your Results
Each tool highlights a different part of your sleep health.
Insomnia Severity Index (ISI): Shows the presence and severity of insomnia, from mild sleep difficulties to more persistent insomnia symptoms.
STOP-BANG Questionnaire: Estimates your risk for sleep apnea (OSA) based on factors like snoring, tiredness, and other physical indicators.
Epworth Sleepiness Scale (ESS): Measures your daytime sleepiness, showing how likely you are to doze off during daily activities.
Your scores show whether you may be at risk for insomnia, sleep apnea, or COMISA. High scores on both insomnia and sleep apnea screenings may suggest COMISA.These results aren’t a diagnosis, but they’re an important first step in understanding your sleep health.
Because of its complexity, co-occurring insomnia and sleep apnea (COMISA) requires a different kind of support, one that goes beyond CPAP therapy or basic sleep hygiene tips.

Why COMISA Is So Often Missed
Many clinics treat only one condition, leaving those with both insomnia and sleep apnea without proper support. Without proper diagnosis, and a coordinated approach, the cycle of sleepless nights and daytime fatigue continues.
COMISA is missed not because it's rare, but because traditional care isn't designed to catch both conditions at once. People with COMISA often spend years struggling with poor sleep, bouncing between treatments, that only address part of the problem.
Insomnia symptoms are often mistaken for stress or anxiety, while underlying sleep apnea goes undiagnosed.
Sleep apnea is treated with CPAP or other devices, but insomnia persists, which can feel frustrating and exhausting.
Clinicians often don't screen for both conditions together, so COMISA remains invisible in many standard sleep apnea assessments.
This gap in care perpetuates the frustrating cycle of COMISA. When insomnia and sleep apnea go unrecognised, undiagnosed, or untreated, individuals are:
2× more likely to discontinue CPAP therapy if insomnia is not addressed
More likely to experience chronic fatigue, mood disturbances, and fragmented sleep
2× more likely to report low mood or anxiety
More likely to experience daytime impairment and poorer quality of life
COMISA: The Missing Link between Insomnia and Sleep Apnea?
To truly restore sleep, insomnia and sleep apnea must be addressed together. Treating only one often leaves people stuck in a cycle of restless nights and fatigue. Sleep apnea can trigger insomnia, and chronic insomnia can worsen breathing disruptions.
Common Signs of COMISA Include:
The Good News: COMISA Is Treatable!
With the right approach, better sleep is possible.
Studies show that when both conditions are addressed together, people experience significant improvements in sleep quality, daytime energy, and overall well-being.
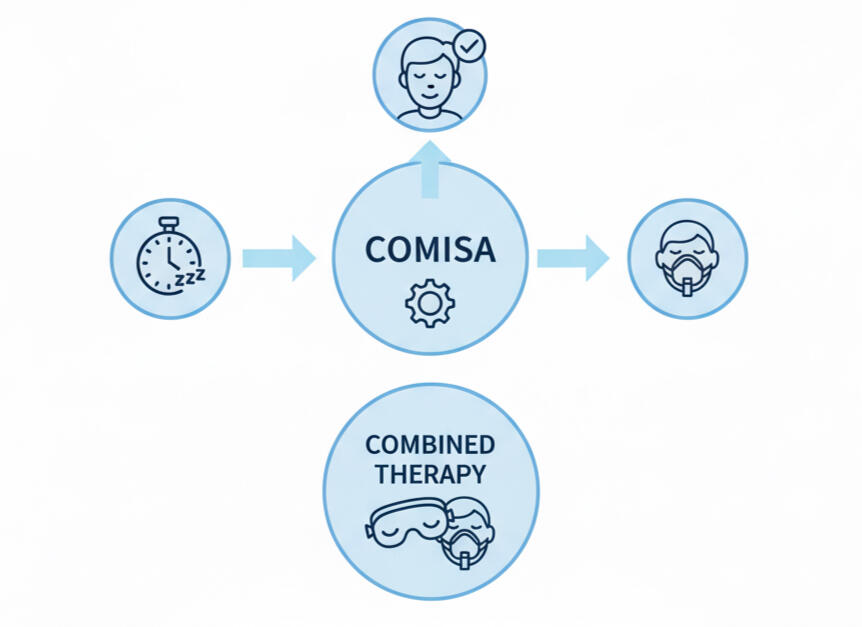
The Secret to Success? A Combined Approach
Current evidence supports a combined treatment model for Co-morbid Insomnia and Sleep Apnea (COMISA), combining Cognitive Behavioral Therapy for Insomnia (CBT-I) with Positive Airway Pressure (PAP) therapy.
By targeting both insomnia and sleep apnea simultaneously, you can achieve more restful sleep and a better quality of life.
CBT-i with PAP-therapy has been shown to:
Reduce insomnia severity by up to 50%
Improve PAP adherence by addressing insomnia symptoms that interfere with consistent use
Enhance sleep efficiency and reduce daytime sleepiness, leading to better mood and cognitive function
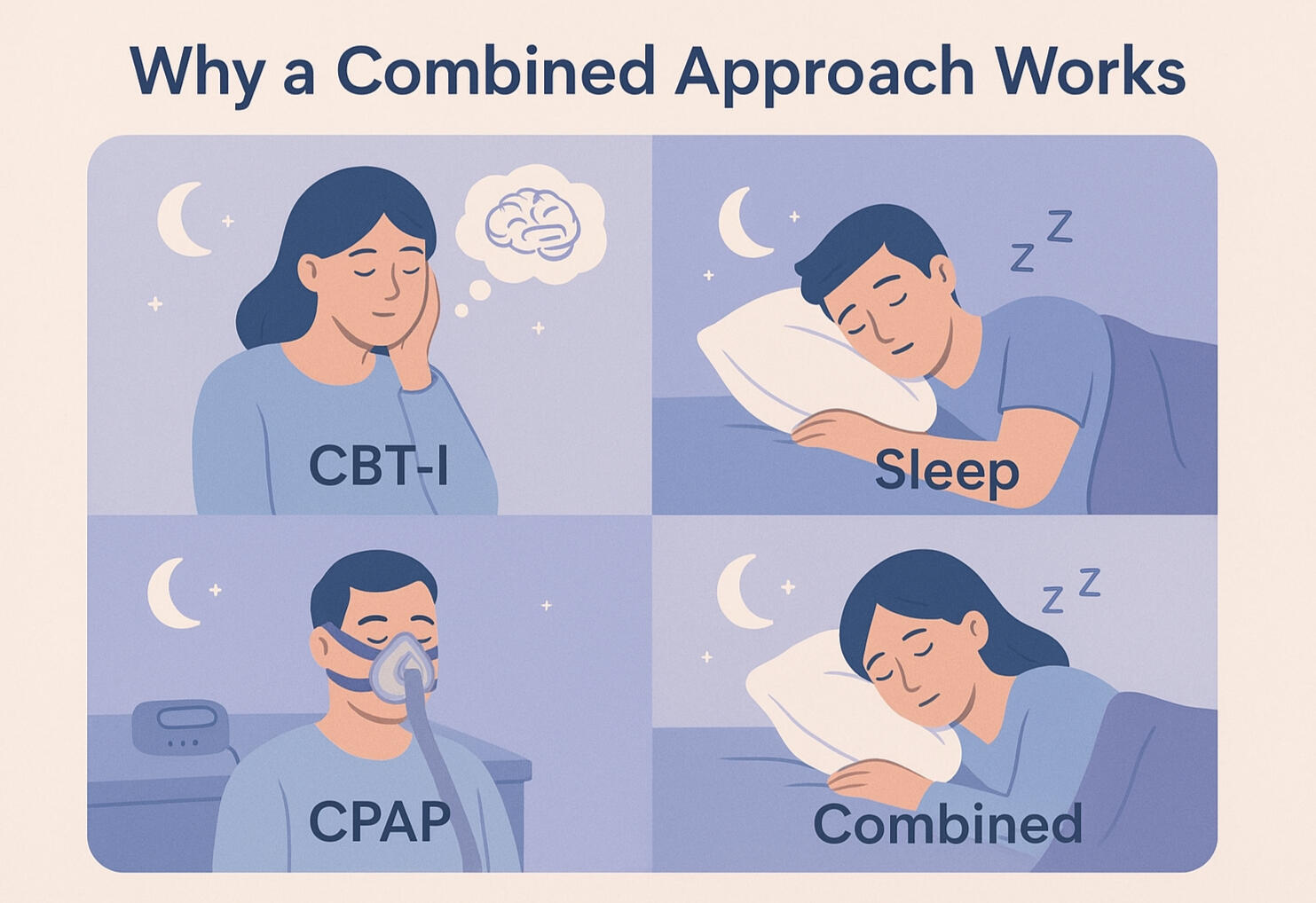
CBT-I targets the root cause of insomnia, helping to quiet anxious thoughts and address behaviors that make sleep difficult. Meanwhile, CPAP physically resolves the breathing issues caused by sleep apnea. This dual-approach leads to better sleep quality and makes it easier to tolerate and benefit from CPAP, since the underlying insomnia is no longer a barrier.
Why Its So Effective
Real progress happens when both insomnia and sleep apnea - COMISA - are recognised and treated together through an integrated approach.

Take your first step toward better, more restful sleep today.
Download the COMISA Sleep Reset:
Breathe. Rest. Repeat:
A Step-by-Step Guide to Managing Insomnia and Sleep Apnea (with CPAP).
Designed to give you proven strategies and practical tools you can start using tonight to finally move toward truly restful, restorative sleep.
What’s Inside the Guide:
A step-by-step COMISA treatment plan for insomnia and sleep apnea
Sleep diaries, trackers, and logs to monitor progress and stay motivated
CPAP success strategies, including desensitization protocols for mask anxiety and claustrophobia
A complete 3-week structured mini-program to help you regain restorative sleep
Expert-created cheatsheets, worksheets, and practical tips to support your progress
Also Included:
Printable sleep diaries and tracking sheets. Easy-to-follow worksheets and action plans. Practical CPAP guidance and expert advice to reduce mask anxiety and claustrophobia.
About the Author

Registered Nurse | Sleep Specialist
Created by a specialist sleep nurse with over 11 years of experience helping people overcome complex sleep challenges, and founder of Dose of Rest—a nurse-led sleep clinic providing personalized support for insomnia, sleep apnea, COMISA, and CPAP-related difficulties.

Should Insomnia Be Treated Before Sleep Apnea?
It's a common misconception that treating sleep apnea with CPAP will also resolve a person's insomnia.
A recent landmark study challenges this notion and found that addressing insomnia first can actually improve outcomes for both conditions.The study followed 145 people with both moderate-to-severe obstructive sleep apnea (OSA) and insomnia. One group started with four weeks of Cognitive Behavioral Therapy for Insomnia (CBT-I) before beginning CPAP therapy. The other group went straight to CPAP therapy after a four-week waiting period.

The Results Were Significant
The group that received CBT-I first was 87% more likely to accept their CPAP devices and used them for an average of one hour longer each night.
After six months, those who started with CBT-I saw a 52% improvement in overall insomnia severity (compared to only 35% in the control group).
They also had better improvements in nighttime insomnia complaints and dysfunctional or unhelpful sleep-related thoughts.
According to lead author Dr. Alexander Sweetman, treating insomnia with CBT-I before starting CPAP therapy significantly improved insomnia symptoms and increased CPAP use.
If you have symptoms of both insomnia and sleep apnea, it's crucial to address the insomnia before or alongside starting CPAP. This can lead to greater acceptance and use of your CPAP machine, improving outcomes for both disorders.
Trouble Sleeping - Even with CPAP?

It’s frustrating: You’ve been diagnosed with sleep apnea, started CPAP, but you still can’t sleep!
While a sleep apnea diagnosis can be a relief, starting CPAP therapy does not always guarantee a perfect night's sleep, especially if you have undiagnosed insomnia.As a result, nights can remain restless, and CPAP may feel overwhelming or, at times, even counterproductive! This doesn't mean CPAP isn't working - it means you need support for both conditions.
You're Not Imagining It.
CPAP helps with breathing, but many still can't fall asleep. Insomnia and CPAP resistance are common. COMISA often:
Makes CPAP feel more uncomfortable
Makes it harder to fall asleep with the mask on
May cause you to stop using your CPAP altogether
The Problem?
Most people aren’t told what to do beyond "Use Your CPAP.”

Those with Co-occurring Insomnia and Sleep Apnea (COMISA):
Are twice more likely to stop CPAP therapy if insomnia remains untreated
Often feel as if they are doing something wrong, or that CPAP simply won't work for them.
Suffer greater physical and mental health challenges than those with either condition alone
Often dread bedtime because they know they won’t sleep
Effective CPAP starts with better sleep. Let’s fix what’s keeping you up... for good!
You're Not Just "a Difficult Case"
These are known parts of the condition, and they are manageable with the right kind of support.

The Clarity You Need for Complex Sleep
Our specialist nurse-led sleep clinic Dose of Rest provides expert care, and integrated strategies for:
We offer personalised consultations, educational resources, and on-demand courses designed to help you better understand and improve your sleep.

Registered Nurse | Sleep Specialist
Learn more about insomnia, sleep apnea, and COMISA—or book your consultation with our specialist sleep nurse today.
Diagnosed with Both Sleep Apnea and Insomnia?
Treating just one doesn’t solve the other. If you have both apnea and insomnia, you need a tailored plan that treats both simultaneously. Learn how with our Breathe + Rest™ protocol.
The BREATHE + REST™ Program
A Fast-Track to Better Sleep
The BREATHE + REST™ Program is a 6-week digital course for people with COMISA—co-occurring insomnia and sleep apnea. Get step-by-step guidance, practical tools, and expert strategies to improve sleep, manage insomnia, and optimize CPAP therapy—whether you’re new or experienced.

This program combines education, actionable exercises, and ongoing support to help you build lasting sleep habits. By following the structured plan, you can regain restorative sleep, feel more energized, and take control of your nights.
Breathe. Rest. Repeat.
Insomnia... But Something Feels Off?
Do you or your partner notice loud snoring, choking, or gasping during sleep? You may have undiagnosed sleep apnea.If you feel excessively sleepy during the day, have trouble staying awake while driving or at work, or experience high blood pressure or heart issues, speak with your doctor or healthcare provider promptly.Undiagnosed and untreated sleep apnea carries serious risks. When insomnia and sleep apnea occur together (COMISA), the likelihood of physical and mental health problems—and even mortality—is higher than with either condition alone.
Using a Dental or Mandibular Advance Device but Still Can't Sleep ?
Mandibular Advancement and Dental Devices improve airflow — but don’t solve sleeplessness or insomnia. Learn simple, effective strategies that actually help. Download our free PDF guide, it's packed full of expert tips to tackle insomnia and improve sleep. Or book a consultation in our sleep clinic Dose of Rest. We offer CBT-i based interventions and programs - the gold standard of care and treatment for insomnia.
Feel Claustrophobic or Anxious with CPAP?
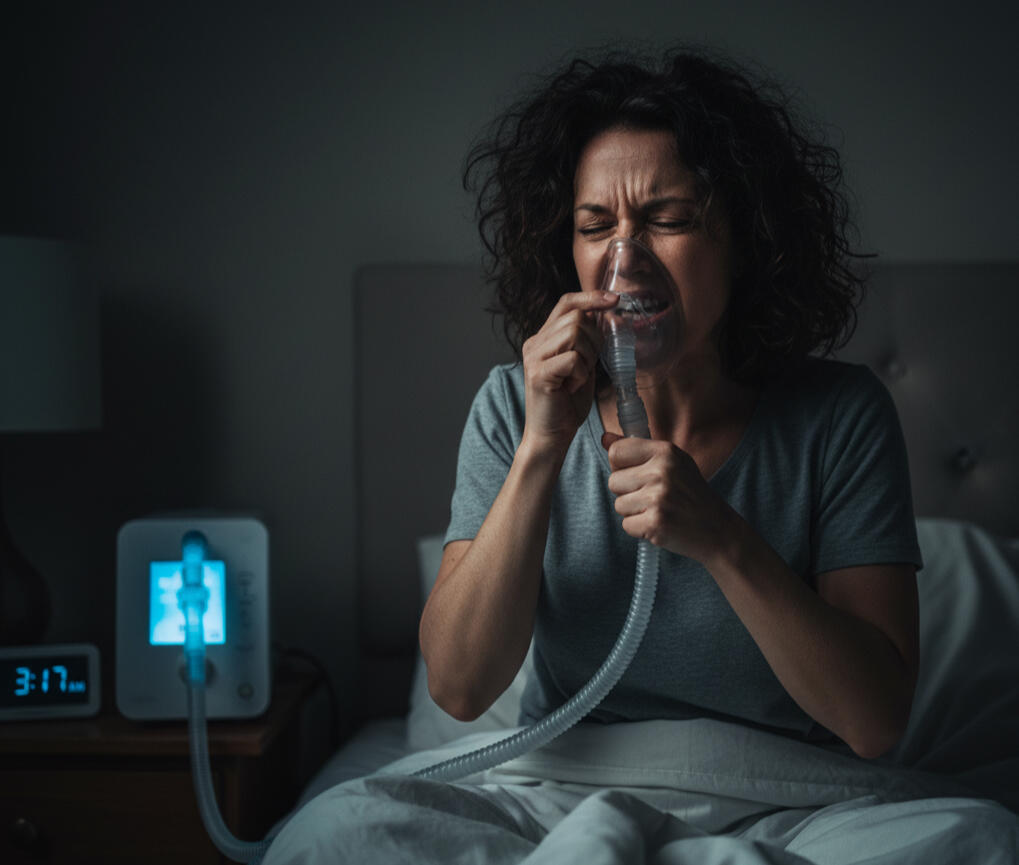
If you feel trapped, claustrophobic or anxious about your CPAP therapy, you're not alone. CPAP intolerance can trigger or worsen insomnia, but there are ways to make it easier.Receive gentle, expert CPAP support from our specialist nurse at Dose of Rest, with over a decade of experience helping patients improve their sleep therapy.
Let's Talk Sleep
Not sure which sleep solution is right for you?
Whether it’s insomnia, sleep apnea, COMISA, or CPAP support, you don’t have to navigate sleep challenges alone.Reach out today by filling out the form below, and we’ll respond shortly.

Evidence-based care and specialist support for Insomnia, Sleep Apnea, and the unique overlap of COMISA.
© 2025 Breathe + Rest™ | sleepapneainsomnia.com | [email protected]